"Wow!"
I looked at the photograph sitting on the table. The edges were slightly frayed. "The belt is funny—I can't believe anyone would just carry that thing around," I said.
"How else do you think we listened to Bon Jovi?" my mom scoffed.
I grabbed the photo and nodded. The cassette tapes piled up on the chair. Last weekend my mom asked me to purge the garage.
Later that evening, we drove to Target. My phone connected with Apple CarPlay. I tapped the Spotify button on the screen.
"...Whooah, we're halfway there..."
The way people consume music has evolved:
In the 1960s, the cassette deck was introduced and it was—and still is—one of the most mechanically complex audio playback formats there ever was. Then in 1980, portable audio players came to the mass market and allowed people to listen to music on the go.
As the story above illustrates, people have moved on to stream their favorite tunes from phones or laptops using software—a format best-suited to keep up with busy lifestyles.
But in healthcare, most teams are stuck playing in the past
Instead of turning to modern platforms or software, people are still operating with outdated credentialing workflows. The data in this report supports this idea:
- 52% of healthcare teams rely on entirely manual credentialing processes.
- 46% of teams do their credentialing work—gathering and verifying vast amounts of provider data—by hand.
- 84% of credentialing teams experiencing turnaround times of 15 days or more.
Credentialing workflows are complicated, but every day spent waiting on credentialing is when a provider isn’t seeing patients—and delayed patient care and reimbursement comes at a high prices for healthcare organizations—up to $10,000 each day.
The good news is 53% of healthcare teams say they are ready for a change to meet their operational goals and the broader mission of enhancing patient care through faster provider readiness.
Modern digital platforms are extremely consistent
More resilient and efficient approaches to credentialing are within reach through modern platforms and credentialing automation.
Benefits of dropping the needle on credentialing automation
Speed and efficiency:
Automated credentialing workflows can turnaround results in record time and with 99.9% verification accuracy rates.
Compliance:
Credentialing automation workflows can guarantee NCQA-compliant files ready for review in about a day. This means faster file delivery that's ready for committee review—2.5x quicker than in-house solutions—helping to eliminate compliance risks.
Flexibility and integration:
Switching between spreadsheets or manually tracking data slows you down. A single platform keeps detailed and up-to-date provider data at your fingertips. The best credentialing software seamlessly integrate with existing workflows and guarantees consistent credentialing, helping healthcare teams save over 500,000 administrative hours in task time.
Fast-forward to modern credentialing
The transition from outdated manual credentialing to modern automated systems isn't just a change—it's an upgrade that healthcare teams need to make to keep pace with the demands of modern patient care.
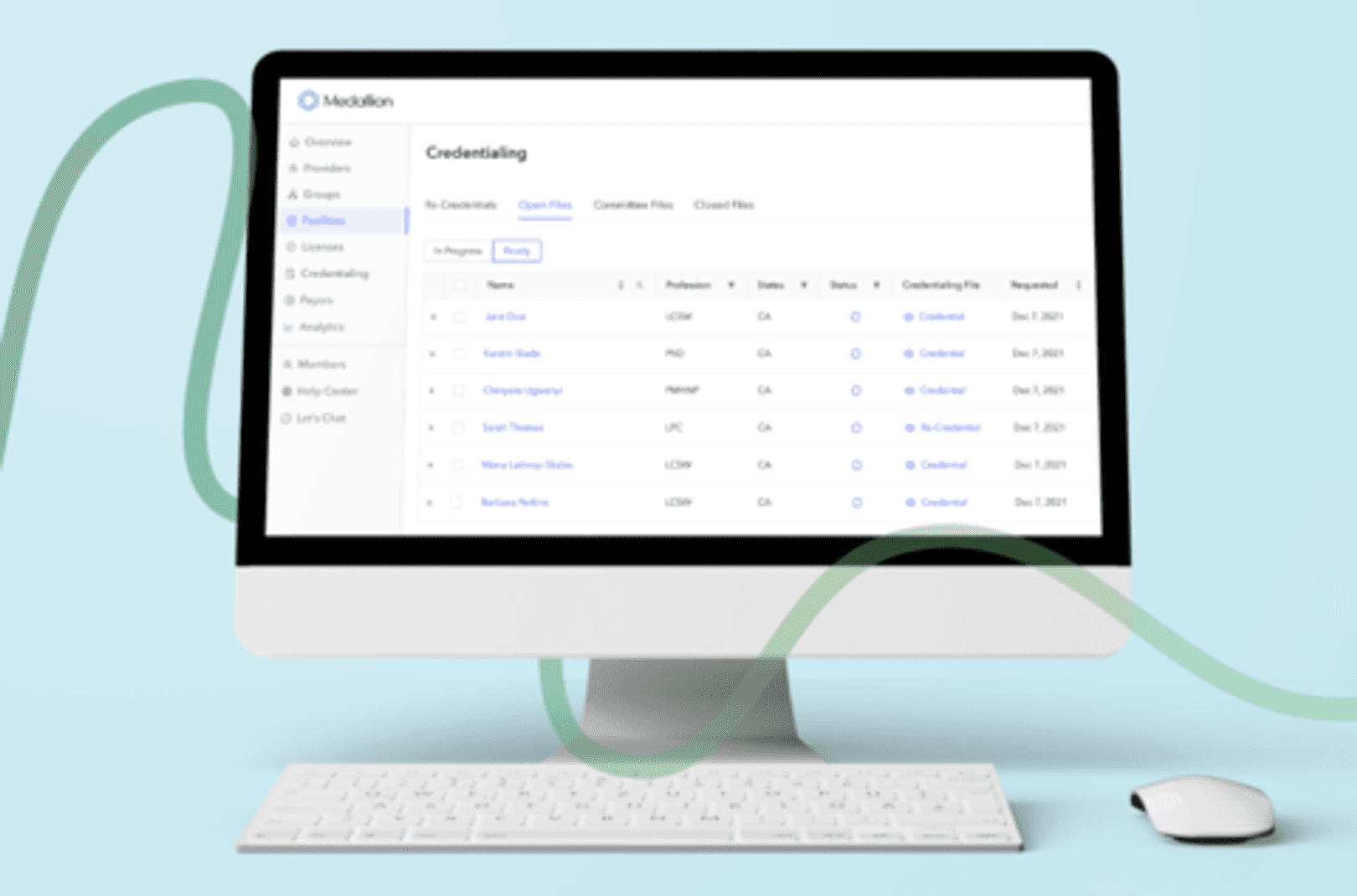
Medallion is leading this transformation, ensuring that your credentialing process is as new-school and efficient to ensure your success.
This has more information about Medallion's credentialing automation solutions and platform—and if at any point you decide you’d like to see it in action, simply get in touch with us.
*Disclaimer: The comparisons on this page are based on information available and accurate as of the date of publication. However, business models, features, capabilities and offerings are subject to change over time.