Better operations starts now
Provider onboarding, credentialing, and enrollment — fully automated
Accelerate time-to-revenue, reduce administrative overhead, and ensure every provider is ready to deliver quality care.



















BEHIND THE TECHNOLOGY
Built on deep expertise, designed to move faster
Decades of credentialing and enrollment expertise, transformed into automation that understands the rules, exceptions, and nuances your team navigates every day.
Results you can count on. Relief your team feels immediately.
When providers are stuck in limbo, care is delayed, revenue slows, and teams burn out trying to move things forward. Medallion changes this with intelligent automation, industry expertise, and SLA-backed delivery, so you can grow without friction.
Get providers seeing patients faster
Automated credentialing and enrollment gets providers in-network quickly, so they can start delivering care instead of waiting on paperwork.
Accelerate revenue, reduce delays
From faster verifications to seamless payer follow-ups, Medallion removes roadblocks that slow down reimbursements and cash flow.
Scale with confidence
Intelligent workflows handle the busywork, from data entry to email parsing to document checks, so your team can focus on what matters most.
50%
average reduction in operating costs
3.5x
faster than legacy CVOs
78%
less time on operational tasks
Powering healthcare organizations to scale
- Tampa General Hospital
- Equip
- Family Care Center
- Headspace
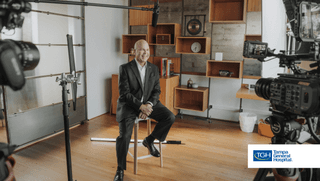
Tampa General Hospital
Equip
Family Care Center
Headspace
Tampa General Hospital
Equip
3300+
license requests
9
months, 50 state expansion
1
central platform to manage provider operations
Family Care Center
100%
score received from Optum
19
days faster to onboard providers
1
platform to manage it all
Headspace
95%
score received on all credentialing audits
60%
less time spent credentialing providers
100M
app downloads globally
Clinical excellence at scale: Automation meets oversight — a new standard for credentialing and enrollment
Leading healthcare organizations move faster, stay compliant, and scale revenue without scaling headcount.
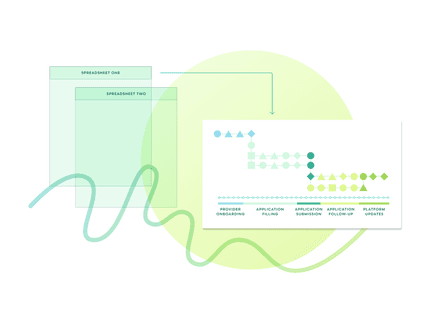
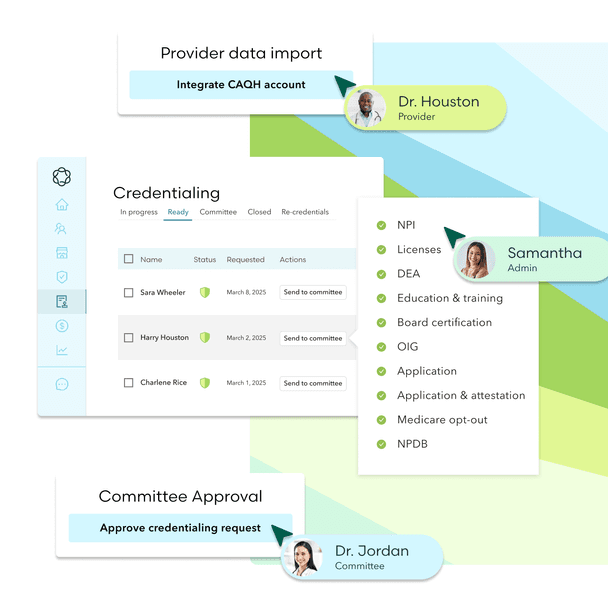
Workflow orchestration that gets smarter over time
Every credentialing or enrollment journey is different. With Medallion, tasks are automatically sequenced based on provider type, state, payer, and historical performance. Our AI-powered platform continuously learns and improves, accelerating speed and accuracy at scale.
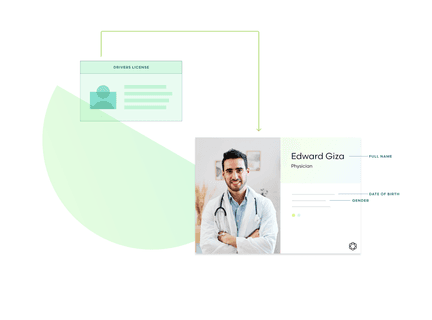
Data extraction, from onboarding to application mapping
Automatically extract data from even the most complex documents — licenses, IDs, certifications, and more. Medallion standardizes everything automatically, so your team doesn’t have to.
Forms and follow-ups that keep things moving
Forms get filled, statuses get tracked, and payer follow-ups happen automatically. No bottlenecks, no chasing, and no added overhead.
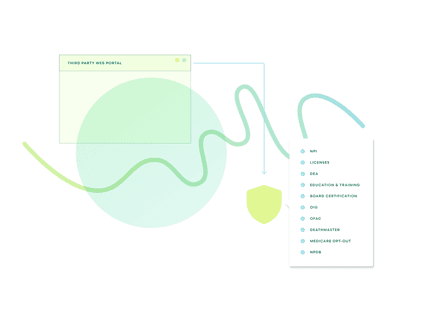
Primary source verifications, built for audit-readiness
Manual checklists are a thing of the past. Primary source verifications are verified automatically, with expert oversight ensuring speed, accuracy, and compliance every time.
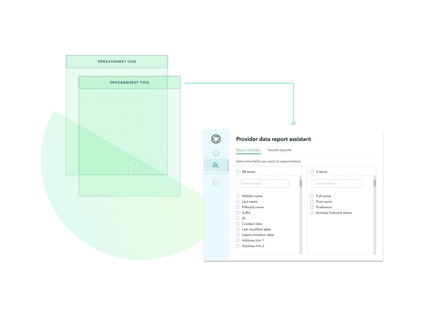
Data transformed, insights you can act on
Every action is logged and structured, powering dashboards that highlight blockers, surface performance trends, and inform smarter decisions. This is more than analytics—it’s operational intelligence that drives ROI.