Speed up payer enrollment with less clicks and fewer rejections
Move from enrollment request to 'in-network' status with government or commercial payers all on one end-to-end platform.
Medallion works with hundreds of














Experience expedited enrollments without sacrificing accuracy
50%reduction in turnaround times.
6(median) business days from request to provider application submission.
25,500+provider enrollments completed.
Enrollments: Quick, visible, accurate.
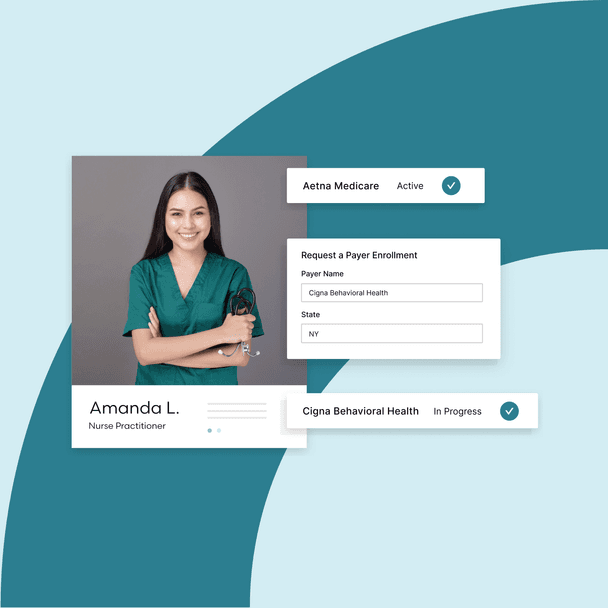
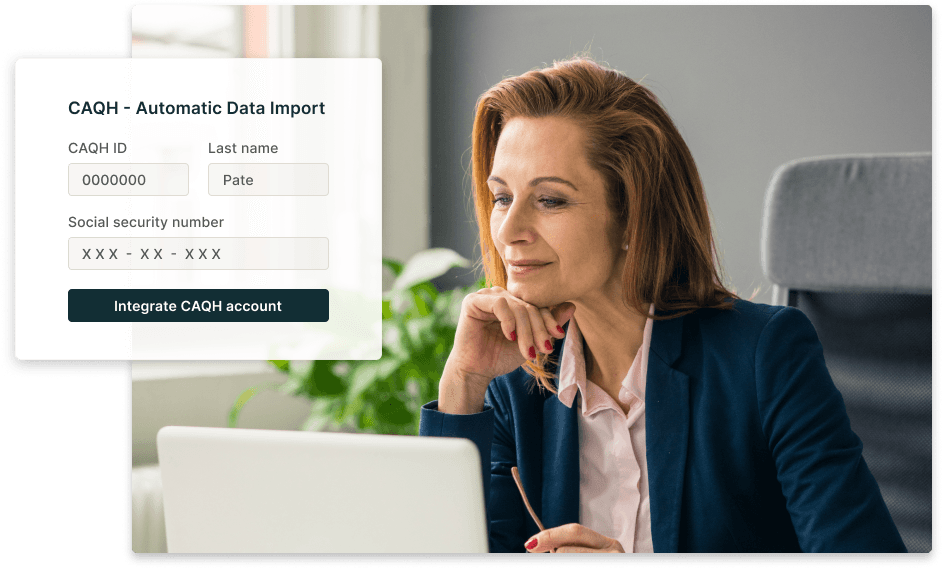
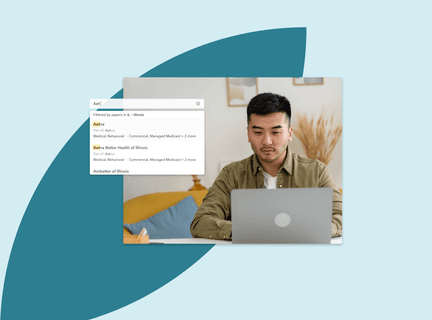
Onboarding
Skip the hassle of starting from scratch
Break new ground with payers with streamlined enrollment using our single provider onboarding flow. Maximize your reach in minimal time with our automated mapping of provider data.
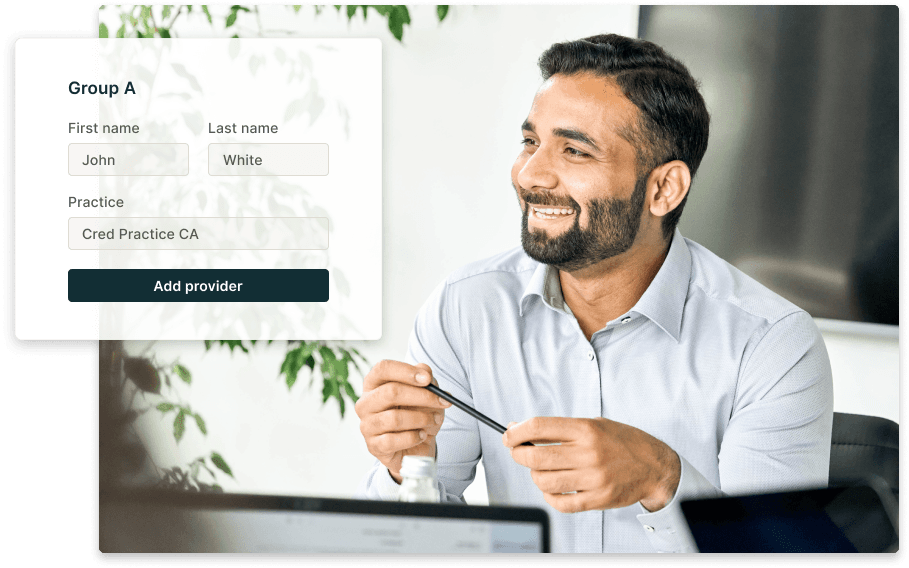
Network linkages
Navigate network complexities with ease
Save time by associating Providers, Groups, and Practice affiliations. Once a relationship is created, it will automatically apply moving forward - doing the heavy lifting on your behalf.
Enrollment status tracking
Experience full-time insight, zero guesswork
Get complete visibility into enrollment progress, including what’s blocking enrollments or delaying requests at any time. Access a dashboard of key enrollment data including payer, state, provider, lines of business, and more and get instantly notified when there’s an update to your enrollment status.
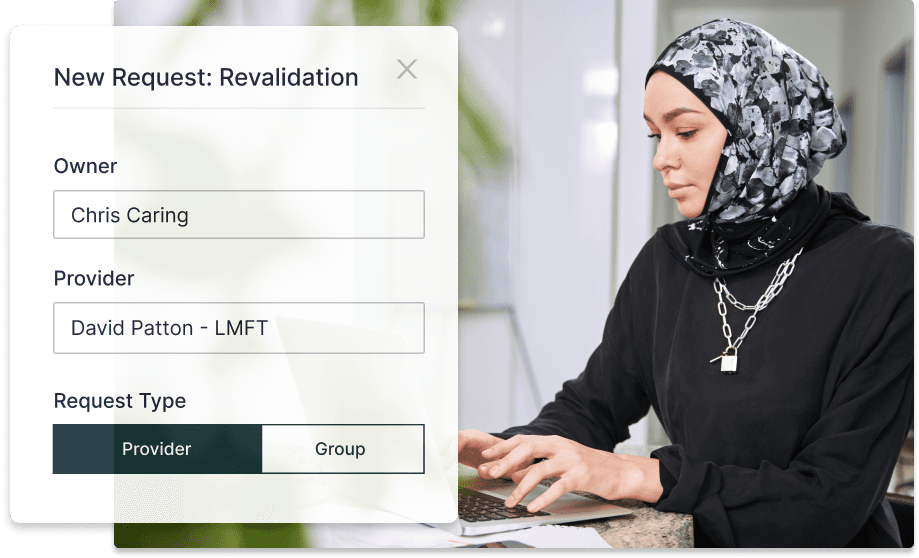
Revalidations
End-to-end enrollment for maximum reimbursement
Re-validate existing enrollments in just a few clicks and track progress effortlessly.
Unlock more revenue opportunities in less time
Experience speed without sacrificing accuracy
Get notified — right when it matters
In order to continue launching in new states, Medallion was the right solution to help us efficiently grow.
Curai Health Team
Medallion's platform is very intuitive, and we have very few providers reaching out asking for help.
Matthew Ortiz Vice President of Payor Strategy and Relations
I would recommend Medallion to anyone in clinical operations.
Irina Shtemler Clinical Network Operations Lead
Medallion tracks our data and ensures we’re compliant with all requirements—it has allowed us to score over 95% on all credentialing audits.
Katie Dave Director of Partner Operations
Our providers like that they only have to operate in one place, and we ask them fewer questions, so they can focus on patient care.
Colleen Wham Director of Business Services

