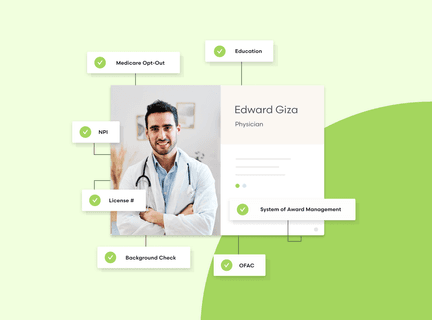
Unify provider credentialing, enrollment and monitoring in one platform
Reduce task time by 71%, slash verification times in half and end risk. Get what you need to run your provider network without any of the back and forth.
Medallion works with hundreds of














Medallion: Better outcomes at lower costs
50%Reduction in operating costs
78%Faster operating speed with a 99.9% accuracy rate
$1.23MPotential revenue gained
Simplify and unite every part of your provider operations
Onboarding
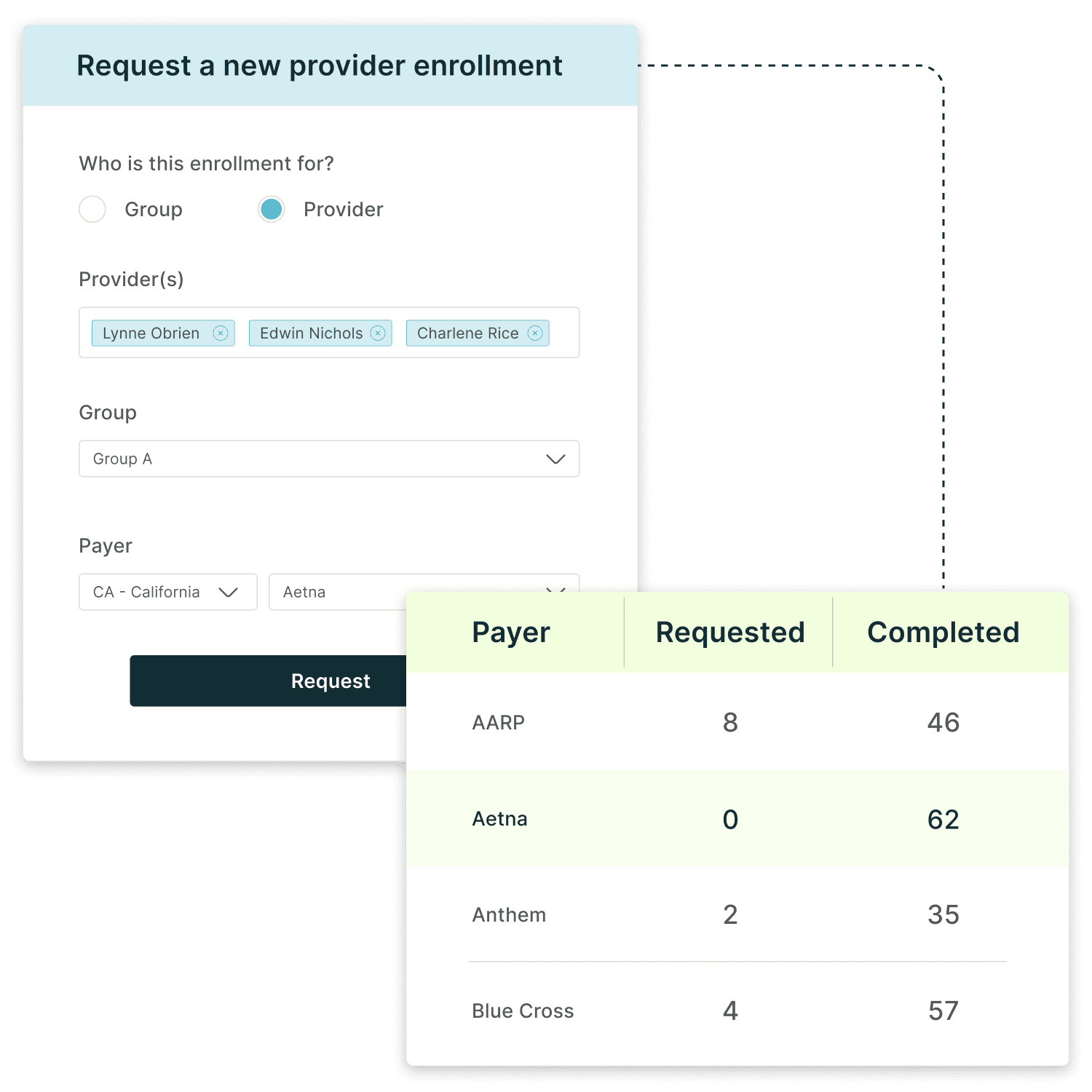
Enrollment workflows
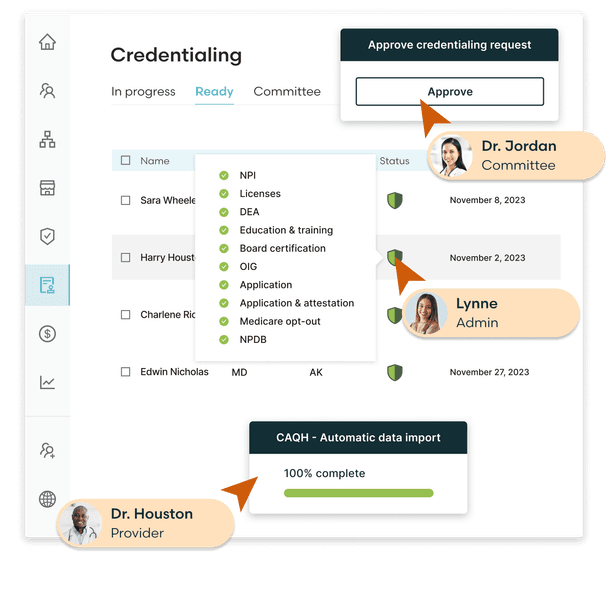
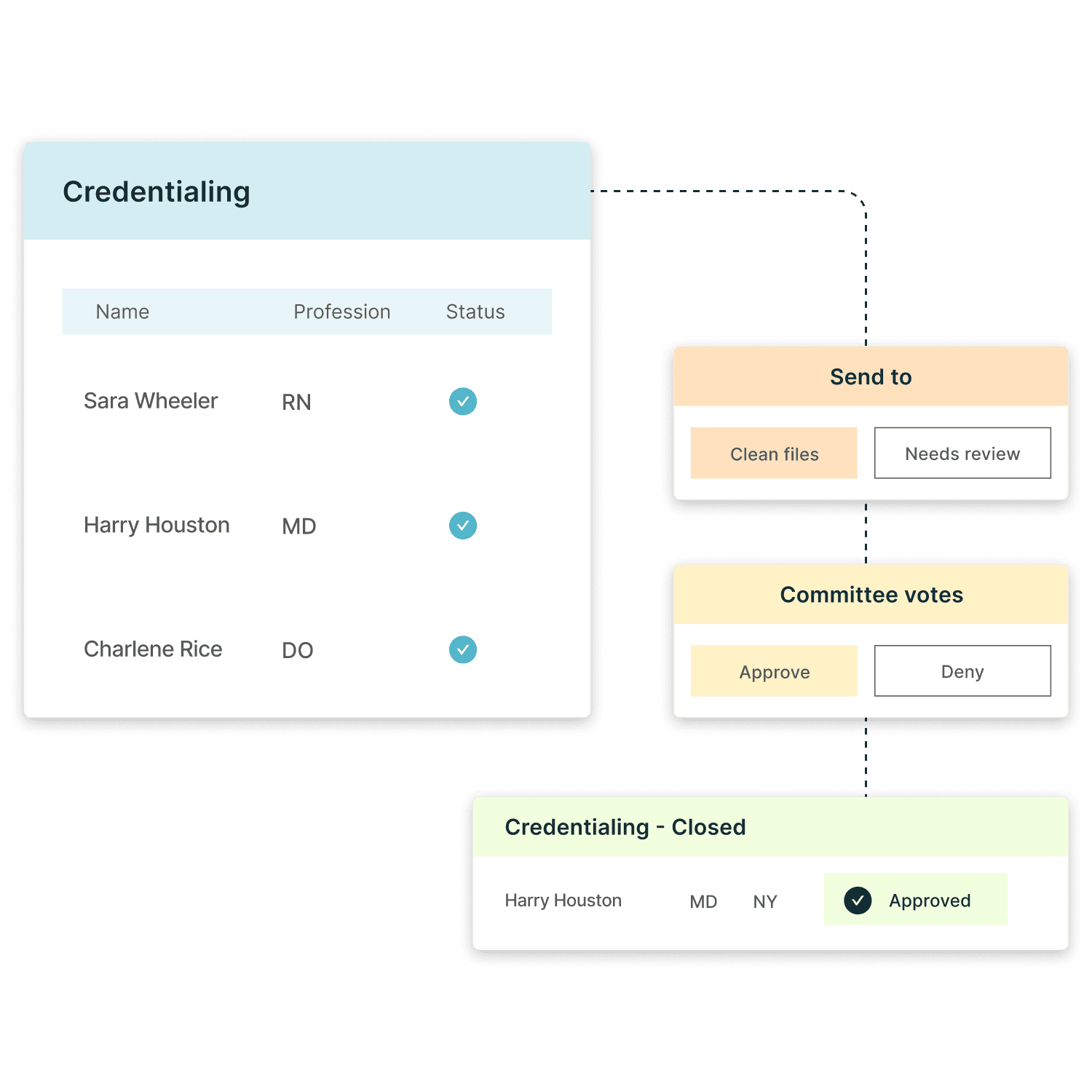
Credentialing workflows
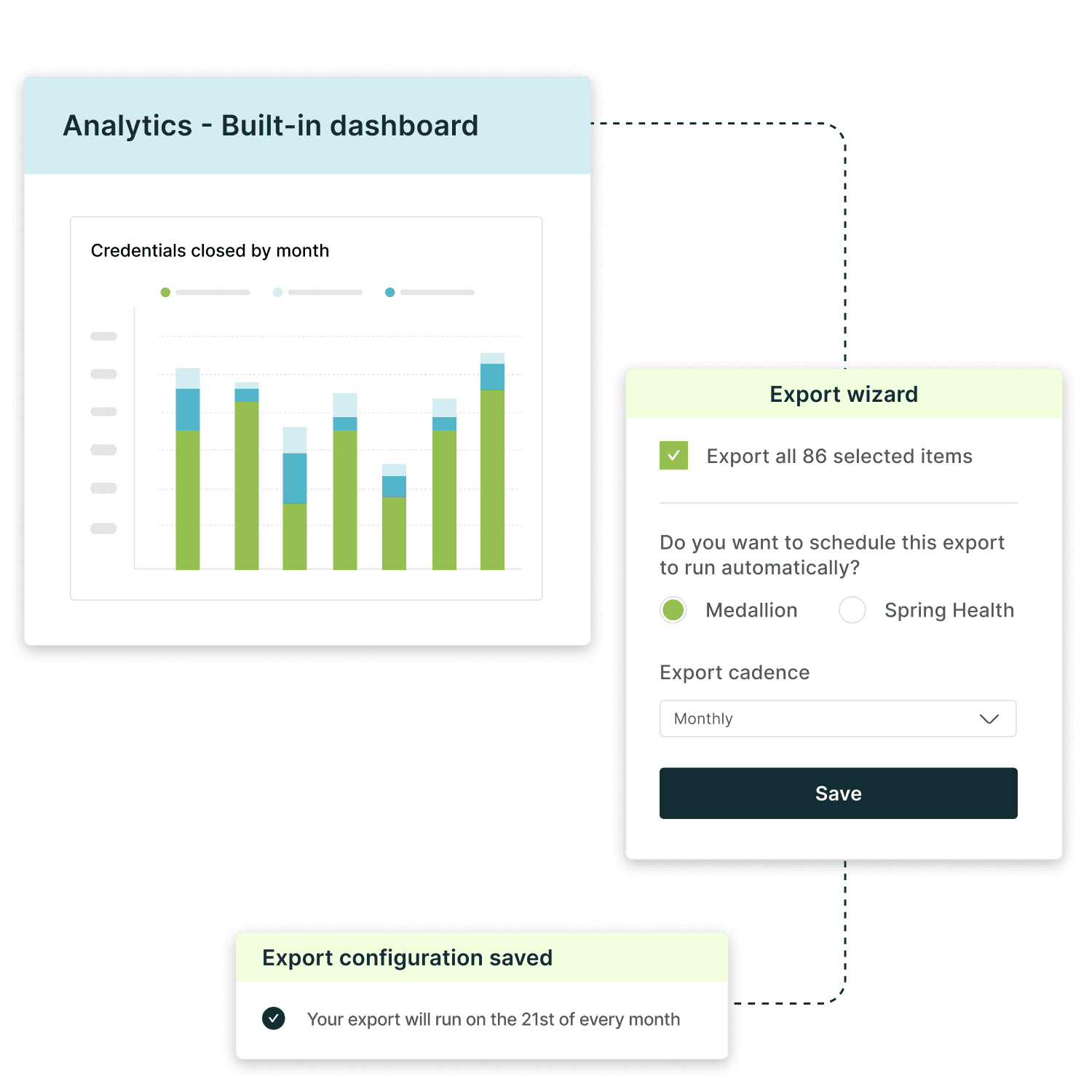
Reporting
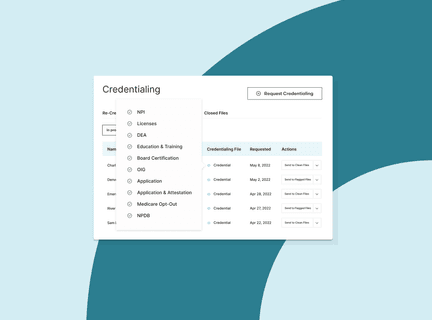
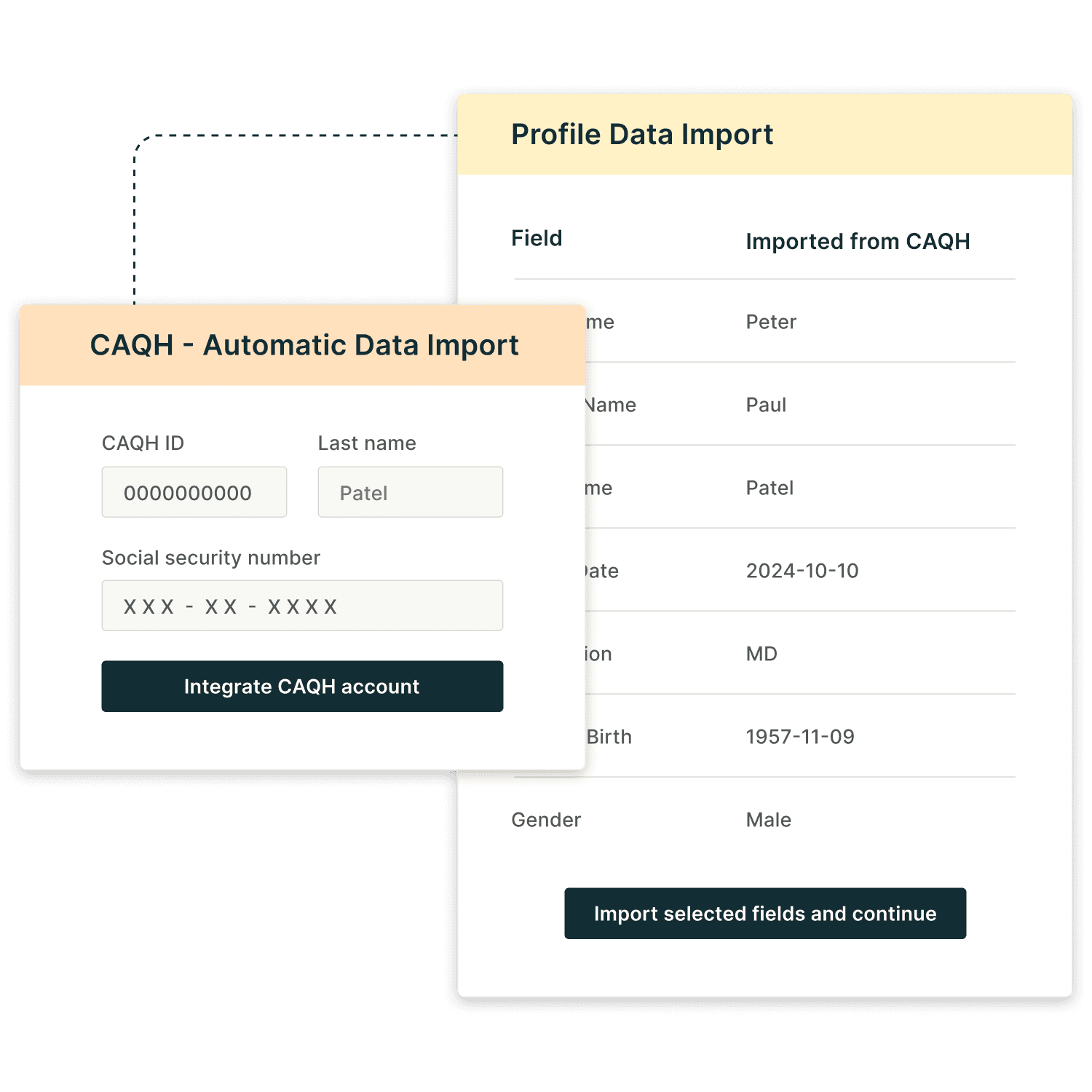
Extend credentialing beyond "instant"
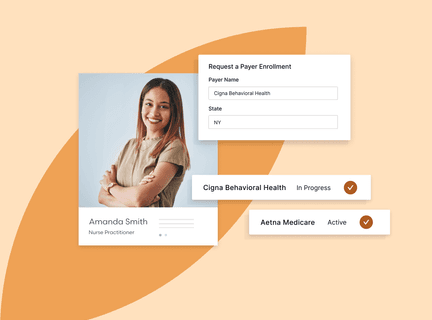
Convert more applications into revenue opportunities
I would recommend Medallion to anyone in clinical operations.
Irina Shtemler Clinical Network Operations Lead
Medallion's platform is very intuitive, and we have very few providers reaching out asking for help.
Matthew Ortiz Vice President of Payor Strategy and Relations
By moving data into Medallion we have one central place. It’s the home where our operations team goes to make sure we have enough people licensed in each state. And it’s the way that we keep patients safe.
Erin Parks, Ph.D. Co-Founder, Chief Clinical Officer
Medallion tracks our data and ensures we’re compliant with all requirements—it has allowed us to score over 95% on all credentialing audits.
Katie Dave Director of Partner Operations
The inefficiency we were experiencing was unsustainable. High operating costs and long timelines risked service quality and our competitive edge. Our clinicians and patients deserved better.
Scott Arnold Executive Vice President & Chief Digital and Innovation Officer
Less busywork, more clarity
A cohesive, powerful easy-to-use platform
Free up provider task time by 250%
Medallion helps you increase retention and revenue with a real-time, transparent and understandable process, without the pain of building it yourself.

